The integration of 3D printing in dentistry is revolutionizing patient care by enabling precise, efficient, and cost-effective solutions that traditional methods struggle to achieve. The dental 3D printing market is experiencing rapid growth, with industry reports indicating an annual growth rate of 17%, projected to reach $930 million by the end of 2025.
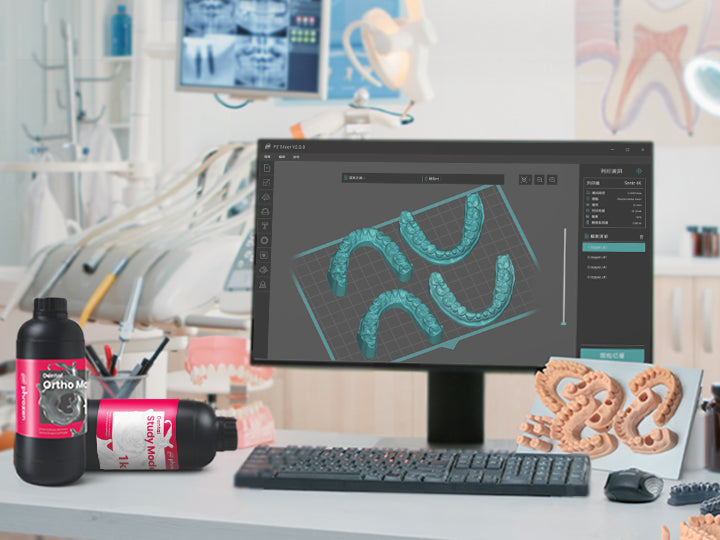
From customized crowns and bridges to patient-specific implants and orthodontic devices, additive manufacturing is redefining how dental professionals design and manufacture restorations. The technology's ability to streamline workflows and reduce turnaround times is a key driver of adoption—more than 50% of dental laboratories have already integrated 3D scanners and CAD/CAM systems, and 20% have implemented 3D printing.
Dentistry has long relied on subtractive manufacturing methods, such as milling, which involve carving restorations from a solid block of material. While effective, these methods are limited by material waste, longer production times, and design constraints.
In contrast, 3D printing constructs dental components layer by layer, allowing for greater precision, minimal material waste, and faster turnaround times. Initially adopted for diagnostic models, 3D printing has now expanded into prosthodontics, orthodontics, implantology, and even maxillofacial surgery.
This article explores the evolution, applications, and advantages of 3D printing in dentistry, while also addressing current challenges and future innovations shaping the industry.
The Evolution of 3D Printing in Dentistry
From Models to Full Restorations: A Timeline of Advancements
3D printing was first introduced in the 1980s and has since evolved into a widely adopted technology across industries such as aerospace, automotive, and healthcare. Dentistry was among the earliest adopters of computer-aided design and computer-aided manufacturing (CAD/CAM), initially using milling machines to create crowns, bridges, and prosthetic frameworks.
However, milling had limitations:
- It wasted a significant amount of material, increasing costs.
- It could not produce intricate internal structures, restricting design capabilities.
- It required specialized tools, which limited flexibility in production.
In the early 2000s, dental laboratories and clinics began integrating stereolithography (SLA) and digital light processing (DLP) printers, allowing for resin-based dental models and temporary restorations. By the 2010s, selective laser melting (SLM) and selective laser sintering (SLS) enabled the direct fabrication of metal dental implants and frameworks, further expanding the scope of 3D printing applications in dentistry.
Today, dental 3D printing has reached a stage where full zirconia crowns, titanium implants, and even bioengineered dental tissues are being explored. The shift toward fully digital workflows—from intraoral scanning to direct 3D printing of restorations—is setting a new standard in dental treatment.
Key 3D Printing Technologies Used in Dentistry
Modern dentistry utilizes a range of advanced 3D printing technologies, each tailored to specific applications, materials, and precision levels. From resin-based printing for detailed crowns and aligners to metal additive manufacturing for durable implants, these technologies are transforming digital dentistry.
Selecting the right 3D printing method depends on factors such as accuracy, speed, material compatibility, and intended use. The table below provides a comparison of the most widely used dental 3D printing techniques, outlining their key advantages and limitations.
Stereolithography (SLA) & Digital Light Processing (DLP)
Stereolithography (SLA) and Digital Light Processing (DLP) are two of the most widely used high-precision 3D printing technologies in dentistry. They are ideal for producing dental models, temporary crowns, and surgical guides. Both rely on photopolymerization, where a UV or laser beam hardens liquid resin layer by layer until the final shape is achieved.
How It Works
The primary difference between these two methods lies in how they cure the material. SLA printers use a single-point laser, ensuring extreme accuracy and fine detail, making them ideal for intricate dental restorations. In contrast, DLP printers project entire layers at once, allowing for faster printing while maintaining high precision. This makes DLP an efficient choice for applications requiring multiple prints in a single batch.
Applications in Dentistry
SLA and DLP are widely used in dental laboratories and clinics for a variety of applications. Dental models created through these technologies aid in treatment planning and patient education, helping both dentists and patients visualize cases before restorations or surgery. Surgical guides printed with SLA or DLP assist in precise implant placement, enhancing accuracy and reducing surgery time. Additionally, temporary restorations such as provisional crowns and bridges can be printed for trial fittings, ensuring proper fit and aesthetics before final fabrication.
Advantages
One of the biggest advantages of SLA and DLP is their high precision, producing smooth surfaces and intricate details, which is essential for dental applications requiring aesthetic and functional accuracy. DLP printing also offers faster production times, as it can print multiple models at once, improving efficiency in dental labs. Furthermore, these technologies allow dentists to create trial restorations, enabling both professionals and patients to evaluate the fit before committing to permanent solutions.
Limitations
Despite their advantages, SLA and DLP have some limitations. The materials used in these processes are limited to light-cured resins, which may not be as durable as final ceramic restorations. Additionally, post-processing is required after printing—models must be cleaned, UV-cured, and sometimes coated to enhance strength and longevity. While these extra steps add to the workflow, the precision and efficiency of SLA and DLP make them indispensable in modern digital dentistry.
Choosing the right 3D printing resin is essential for achieving high precision in dental applications. Different resins cater to specific needs, such as study models, crown and bridge restorations, and gingiva masks. If you’re unsure about which resin suits your workflow best, check out our comprehensive guide on Phrozen Dental Resins for detailed insights on selecting the optimal material.
Selective Laser Sintering (SLS) & Selective Laser Melting (SLM)
Selective Laser Sintering (SLS) and Selective Laser Melting (SLM) are advanced 3D printing technologies used in dentistry, particularly for metal dental implants, partial denture frameworks, and high-strength prosthetics. These methods utilize powder-based materials and high-powered lasers to create precise and durable dental restorations.
How It Works
Both SLS and SLM employ laser-based fusion to transform powdered materials into solid dental components. SLS works with polymer-based powders, commonly used for temporary models or guides. In contrast, SLM is dedicated to metal fabrication, making it a preferred choice for permanent dental restorations, implants, and metal prosthetics. The laser selectively melts or sinters the powder, layer by layer, forming strong, detailed structures.
Applications in Dentistry
SLS and SLM are widely used for producing customized and biocompatible dental solutions:
- Titanium Dental Implants: 3D-printed implants can be tailored to fit a patient’s jawbone structure, enhancing osseointegration (bone bonding) and long-term stability.
- Partial Denture Frameworks: Metal frameworks for removable dentures can be precisely printed, eliminating the need for manual wax casting and improving fit.
- Metal Crowns and Bridges: SLM technology allows dental laboratories to manufacture strong, biocompatible restorations, replacing traditional casting methods with greater efficiency.
Advantages
One of the biggest advantages of SLS and SLM is their ability to directly print metal restorations, eliminating the need for traditional casting or manual shaping. These technologies enable complex geometries, such as lattice structures, which improve implant integration and strength. Additionally, SLM produces restorations with high mechanical strength, making it ideal for long-term dental solutions that require durability and precision.
Limitations
Despite their benefits, SLS and SLM come with some challenges. Industrial-grade metal 3D printers are expensive, making them less accessible for smaller dental labs. Additionally, post-processing is required—printed parts must undergo heat treatment and surface polishing before they can be used in clinical applications. While these extra steps add to the workflow, the superior strength and precision of SLS and SLM make them indispensable for high-performance dental restorations.
Material Jetting (MJ)
Material Jetting (MJ) is an advanced 3D printing technology that is particularly useful for multi-material dental models, prototypes, and full-color anatomical replicas. Unlike other additive manufacturing methods, MJ allows for highly detailed, multi-textured, and multi-colored prints, making it a powerful tool for dental education, surgical planning, and research applications.
How It Works
Material Jetting operates similarly to inkjet printing, but instead of ink, it deposits tiny droplets of photopolymer resin. These droplets are instantly cured by UV light, solidifying the material layer by layer. Unlike SLA and DLP, which work with a single material per print, MJ can print multiple materials simultaneously. This capability allows for the simulation of varying colors, textures, and even hardness levels within a single model, making it ideal for complex dental applications.
Applications in Dentistry
MJ is widely used in dental laboratories and research facilities for producing highly detailed and multi-textured models.
- Full-Color Dental Models: These models help with patient education and case presentations, allowing for better communication between dentists and patients.
- Multi-Material Prototypes: Dental professionals can use MJ to evaluate different materials and textures before final production, ensuring optimal performance.
- Surgical Planning Models: MJ can print lifelike anatomical structures that differentiate between bone and soft tissue, aiding in pre-surgical assessment.
Advantages
One of the most significant advantages of MJ is its ability to print multiple materials in a single model, allowing for realistic simulations of gum tissue, enamel, and bone density. It also offers high precision and ultra-smooth surfaces, making it an excellent tool for detailed visualization and planning. Another benefit is that no post-curing is required, as the material is fully solidified immediately after printing.
Limitations
Despite its advantages, MJ has some drawbacks. Material costs are higher compared to SLA and DLP resins, making it less cost-effective for routine dental applications. Additionally, MJ is not commonly used for final restorations—it is primarily designed for prototyping and model production, rather than functional prosthetics. Some MJ-printed materials may also be brittle, limiting their long-term durability in clinical settings.
Fused Deposition Modeling (FDM)
Fused Deposition Modeling (FDM) is a cost-effective and widely accessible 3D printing technology, primarily used for educational models, training aids, and prototyping in dentistry. While it lacks the precision of SLA, DLP, or SLM, it remains an excellent choice for non-clinical applications, particularly in dental education and research.
How It Works
FDM printers use a heated nozzle to extrude thermoplastic filament, which is laid down layer by layer to construct a solid object. The material melts during extrusion and solidifies upon cooling, allowing for simple yet durable models. Compared to other 3D printing technologies, FDM offers lower resolution and surface smoothness, but it compensates with affordability and accessibility.
Applications in Dentistry
Due to its cost-effectiveness and ease of use, FDM is widely used in dental education, training, and prototyping rather than direct patient care.
- Educational & Training Models: Dental students and professionals use FDM-printed models to practice procedures and refine techniques without risk.
- Orthodontic Demonstration Models: Dentists and orthodontists use FDM-printed models to explain treatment plans to patients, improving communication and understanding.
- Prototyping for Dental Equipment: FDM is useful for designing and testing new dental tools and instruments, allowing manufacturers to refine prototypes before mass production.
Advantages
One of the key benefits of FDM is its low cost and widespread accessibility. FDM printers are significantly more affordable than SLA, DLP, or SLS, making them ideal for budget-conscious dental institutions and training centers. Additionally, FDM supports a wide range of materials, including biodegradable plastics like PLA, as well as durable options like ABS and PETG. Another advantage is its ability to print large-scale models, making it useful for bulk production of educational and demonstration models.
Limitations
Despite its affordability and ease of use, FDM has significant limitations for clinical dentistry. The resolution and accuracy are lower than resin or metal 3D printing methods, making it unsuitable for intricate dental restorations. The surface finish is rough, requiring post-processing such as sanding or smoothing to achieve finer details. Additionally, FDM is limited to thermoplastics, meaning it cannot print in resin, metal, or biocompatible materials, restricting its use to non-clinical applications.
Applications of 3D Printing in Dentistry
The use of 3D printing in dentistry extends beyond prototyping and educational models. Modern dental practices and laboratories are leveraging additive manufacturing to create highly customized, patient-specific restorations, implants, and orthodontic devices. Below are the key applications of 3D printing in dental care, categorized for better clarity.
Restorative & Prosthetic Dentistry
Crowns, Bridges, and Inlays
3D printing has revolutionized the fabrication of dental restorations, such as crowns, bridges, and inlays, by reducing both material waste and production time. Traditionally, these restorations were made using milling machines, which carved structures from a ceramic block. While effective, milling generates excessive material waste and is limited in design complexity.
With the advent of SLA, DLP, and SLS technologies, dental professionals can now print both temporary and permanent restorations with superior precision. These restorations are typically made from light-cured resins, ceramic-infused composites, and hybrid materials, which closely replicate the strength, translucency, and aesthetics of natural enamel.
Applications in Dentistry
The ability to 3D print dental restorations has significantly improved workflow efficiency in dental clinics and laboratories.
- Temporary Restorations: SLA and DLP printers enable the rapid production of temporary crowns and bridges, allowing patients to receive interim restorations on the same day while waiting for a final prosthesis.
- Zirconia and Ceramic Crowns: Lithography-based ceramic manufacturing (LCM) is advancing the field by enabling the direct 3D printing of zirconia restorations, reducing reliance on traditional milling techniques.
- Customized Inlays & Onlays: Dentists can now design and print inlays and onlays that precisely match a patient’s tooth structure, ensuring a perfect fit with minimal adjustments.
3D printing allows for the rapid and precise fabrication of crown and bridge models, reducing turnaround times for dental restorations. Digital workflows ensure an exact fit, minimizing errors and adjustments. If you’d like a practical walkthrough on how to 3D print crown and bridge models with removable dies, you can follow our detailed step-by-step guide here.
Advantages of 3D Printing in Restorative Dentistry
One of the biggest benefits of 3D printing in restorative dentistry is its ability to significantly reduce turnaround time. Same-day restorations are now a reality, eliminating the need for patients to return for multiple appointments. Additionally, 3D printing minimizes material waste, as it only uses the necessary amount of material, unlike milling, which generates significant excess. The digital workflow ensures enhanced accuracy, resulting in restorations with superior anatomical fit and function.
Challenges
Despite its many advantages, 3D printing in restorative dentistry still faces some challenges. Not all dental materials are currently printable—while resins and hybrid composites are widely used, fully printable zirconia and lithium disilicate restorations are still under development. Additionally, surface finishing is required for 3D-printed crowns, bridges, and inlays to achieve the final level of polish, color, and translucency required for aesthetic perfection. This may involve glazing, polishing, or additional curing processes.
2. Orthodontics & Aligners
Clear Aligners & Retainers
3D printing has revolutionized orthodontics, particularly in the mass production of clear aligners. Traditionally, aligners were created through thermoforming over physical models, requiring manual labor and multiple steps. With the introduction of 3D scanning and direct printing, orthodontists can now produce customized aligners faster and with higher accuracy, reducing both costs and production time.
One of the key benefits of 3D-printed aligners is their ability to support personalized treatment plans. Patients receive sequential sets of aligners, each designed to gradually shift teeth into their correct position. Automated 3D printing farms allow for batch production of aligners, significantly reducing manufacturing costs. Additionally, the digital workflow eliminates human error, as scanning and printing replace traditional manual impressions, ensuring a more precise fit for each patient.
Customized Orthodontic Brackets & Expanders
Beyond aligners, 3D printing is also being used to fabricate custom orthodontic components, such as brackets, arch expanders, and indirect bonding trays. With Selective Laser Melting (SLM), orthodontists can print custom metal brackets that provide a better fit and adhesion compared to conventionally manufactured brackets. These customized components improve treatment efficiency by offering higher precision and patient comfort, leading to more predictable orthodontic outcomes.
3D printing has revolutionized the production of clear aligners, making in-house manufacturing more efficient than ever. Clinics can now scan, design, and print models for thermoforming within hours. For a step-by-step breakdown of the entire aligner production process, visit our detailed guide on 3D printing thermoformed clear aligners.
Advantages of 3D Printing in Orthodontics
The biggest advantage of 3D printing in orthodontics is mass customization. Unlike traditional methods, aligners and retainers can be produced in large quantities simultaneously, making it easier for practices to manage multiple patients efficiently. Patients also benefit from fewer clinic visits, as they receive pre-planned sets of aligners, reducing the need for frequent adjustments. Moreover, digital workflows have enhanced the patient experience by eliminating the discomfort of traditional putty-based molds, replacing them with precise intraoral scans.
Challenges
Despite its efficiency, 3D printing in orthodontics requires a significant initial investment. Orthodontic clinics must purchase high-speed resin 3D printers and the necessary software to set up in-house production, which can be costly. Additionally, aligners still rely on thermoformed plastics, meaning they cannot yet be directly printed with final biocompatible materials. While research is advancing, current 3D-printed aligners still require post-processing steps to make them functional.
3. Implantology & Surgical Planning
Dental Implants & Custom Prostheses
3D printing is redefining implant dentistry by enabling patient-specific, precisely designed implants. With Selective Laser Melting (SLM) technology, dental professionals can now print titanium and cobalt-chromium implants that perfectly match a patient’s bone structure, improving long-term success rates.
One of the primary advantages of 3D-printed titanium implants is their customized fit, which minimizes implant rejection and failure rates. Additionally, 3D-printed porous implants promote osseointegration, allowing bone tissue to grow into the implant’s surface, ensuring stronger and more stable integration. As a result, patients benefit from faster healing times, reduced post-surgical complications, and improved comfort.
Surgical Guides for Implant Placement
For precise and predictable implant placement, dentists rely on 3D-printed surgical guides, which are designed using CBCT scans and digital workflows. These guides help ensure the implant is placed at the correct angle and depth, reducing the risks associated with misalignment and surgical complications.
Several types of 3D-printed surgical guides are used in implantology:
- Bone Reduction Guides: Used in cases where alveolar bone reshaping is required before implant placement.
- Stackable Implant Guides: Multi-layered, magnetically connected surgical guides that assist in bone reduction, drilling, and implant positioning with precision.
- Immediate Loading Prosthetics: 3D-printed, implant-retained dentures that allow for same-day implant loading, reducing treatment time and improving patient satisfaction.
Advantages of 3D Printing in Implantology
The ability to create patient-specific implants and surgical guides has significantly improved the predictability and efficiency of dental implant procedures. Custom-fitted implants enhance comfort and longevity, while pre-planned guides reduce complications and minimize surgical time. With digitally designed and 3D-printed surgical templates, dentists can achieve higher precision, leading to better long-term outcomes for patients.
Challenges
Despite its benefits, 3D printing in implantology comes with some challenges. The high cost of SLM machines for metal implant fabrication makes them a significant investment for clinics and dental labs. Additionally, metal 3D-printed implants require extensive post-processing, including heat treatment, surface finishing, and sterilization, before they are ready for clinical use. While these steps add time and cost, the precision and biocompatibility of 3D-printed implants make them a game-changer in modern dentistry.
4. Diagnostic & Educational Models
Anatomical Models for Treatment Planning
3D-printed anatomical models have become essential tools for treatment planning, allowing dentists and oral surgeons to visualize complex cases before performing procedures. These models are created using CBCT scans or intraoral scans and serve as highly accurate replicas of a patient’s oral anatomy. They provide better insight into challenging cases, enabling more precise treatment strategies while also improving patient communication.
Some of the key applications of 3D-printed anatomical models include:
- Full-Color Jaw Models: Printed using Material Jetting (MJ) technology, these models provide bone and soft tissue differentiation, making them valuable for pre-surgical planning.
- Endodontic Training Models: Used by dental students and professionals to practice root canal procedures on lifelike replicas, improving their technique before treating real patients.
- Pathological Models: Designed to study tumors, bone defects, and other oral abnormalities before surgery, ensuring better treatment outcomes.
Patient Education & Case Presentations
For many patients, understanding X-rays and digital scans can be challenging. 3D printing enhances patient education by allowing dentists to create physical replicas of a patient’s teeth, jaw, or affected areas. These models help patients visualize their condition, leading to better comprehension and informed decision-making.
Key benefits of 3D-printed patient models include:
- Improved Case Acceptance: Patients are more likely to approve recommended treatments when they can physically see and touch a model of their own dental issues.
- Training for Dental Students: Universities and training institutions use 3D-printed mandibles, teeth, and skull models to provide hands-on experience to students before they begin clinical practice.
Advantages of 3D-Printed Diagnostic Models
The use of 3D-printed diagnostic models has significantly improved surgical planning and patient communication. Dentists can visualize procedures more clearly, reducing the risk of surgical errors in complex cases. These models also enhance patient trust by offering a tangible representation of their treatment plan, making them feel more confident about the procedure.
Challenges
Despite their benefits, 3D-printed diagnostic models are not always necessary. Some cases, especially routine dental procedures, may not require a physical model, making the cost unjustified. Additionally, high-detail models require specialized resins, which can be expensive, increasing overall treatment costs for clinics and patients.
Advantages and Challenges of 3D Printing in Dentistry
While 3D printing offers groundbreaking benefits in dentistry, it also presents certain challenges that must be addressed before widespread adoption can be achieved. This section explores the key advantages and current limitations of additive manufacturing in dental care.
Advantages of 3D Printing in Dentistry
The adoption of 3D printing in dentistry has introduced efficiency, accuracy, and affordability that traditional methods cannot match. From customized restorations to faster treatment times, the technology enhances both clinical workflows and patient satisfaction. Below are the key advantages of integrating 3D printing into modern dental practices.
1. Customization & Patient-Specific Solutions
One of the most significant advantages of 3D printing in dentistry is its ability to create highly personalized restorations. Unlike conventional manufacturing methods, which rely on standardized molds, 3D printing designs each prosthetic based on a patient's unique oral anatomy. This results in a perfect fit, ensuring greater comfort, better functionality, and long-term durability.
- Perfect Fit: Custom restorations improve aesthetic integration, chewing efficiency, and overall patient comfort.
- Patient-Specific Surgical Guides: 3D-printed implant guides improve accuracy, reducing surgical risks and complications.
2. Faster Turnaround Times
Traditional milling or casting methods require multiple steps and manual labor, leading to longer wait times for restorations. With 3D printing, same-day dentistry is now a reality. Instead of waiting weeks for lab-produced crowns or bridges, dentists can design, print, and place restorations in a single appointment.
- Chairside Restorations: In-office 3D printing enables on-demand fabrication of crowns, bridges, and dentures.
- Reduced Lab Dependency: Dentists with in-house 3D printers can bypass third-party labs, significantly speeding up patient treatments.
3. Cost-Effective Production
3D printing is a material-efficient manufacturing process, unlike subtractive methods like milling, which generate significant material waste. By using only the required amount of material, 3D printing reduces costs and makes dental restorations more affordable for both clinicians and patients.
- Minimized Waste: 3D printing adds material layer by layer, using only what is necessary, unlike milling, which carves out material from a solid block.
- Lower Production Costs: Eliminates the need for expensive molds, manual wax-ups, and traditional casting techniques.
4. Precision & Accuracy
One of the most critical aspects of dental restorations is fit and accuracy. Poorly fitting restorations can lead to bite issues, discomfort, and long-term failure. 3D printing achieves micron-level precision, ensuring a seamless fit and minimal post-processing adjustments.
- Improved Marginal Fit: Reduces gaps between restorations and natural teeth, minimizing failure risks and cement washout.
- Enhanced Surface Detail: Ideal for high-resolution dental prosthetics, orthodontic appliances, and intricate implant structures.
5. Better Patient Experience
With digital impressions, same-day restorations, and reduced chair time, 3D printing significantly enhances patient satisfaction. Patients no longer have to undergo messy traditional impressions or endure multiple appointments for their restorations.
- No More Putty Molds: Intraoral scanning combined with 3D printing eliminates the discomfort of traditional impression materials.
- Fewer Appointments: Patients receive their dental restorations faster, making treatments more convenient and less time-consuming.
Challenges of 3D Printing in Dentistry
While 3D printing has transformed dentistry, there are still several limitations and challenges that must be addressed before the technology can fully replace traditional manufacturing methods. These challenges primarily revolve around material limitations, post-processing requirements, costs, and regulatory concerns.
1. Limited Material Availability
Although 3D printing materials have advanced significantly, not all dental materials are available in printable form. Traditional restorations, such as zirconia and lithium disilicate crowns, are still primarily milled because ceramic 3D printing technology is still developing. Furthermore, some resins used for 3D-printed restorations lack the durability and wear resistance of conventional materials, making them less ideal for long-term restorations.
- Ceramic 3D Printing is Still Developing: Zirconia and lithium disilicate restorations remain milled rather than printed, limiting the range of materials available for direct 3D printing.
- Material Strength Concerns: Some 3D-printed resins are less durable than traditional materials, making them prone to wear and fracture over time.
2. Post-Processing & Finishing Requirements
Unlike milled restorations, which often require minimal post-processing, most 3D-printed dental prosthetics need additional finishing steps before they can be used. Depending on the material and printing method, this may include curing, sintering, polishing, or surface treatments to achieve the necessary strength and aesthetics.
- Curing & Sintering Required: Resin-based restorations must be post-cured under UV light, while metal-printed parts need heat treatment and surface finishing before use.
- Surface Finishing Needed: Printed restorations often require additional glazing, veneering, or sanding to achieve a smooth surface and natural-looking finish.
3. High Initial Investment
While 3D printing can reduce long-term costs, the upfront investment required for industrial-grade machines, software, and training is significant. High-quality metal and ceramic 3D printers are expensive, making them unaffordable for smaller dental clinics. Additionally, dentists and lab technicians must be trained in 3D design software and machine operation, adding to the overall investment.
- Expensive Industrial Machines: High-end SLM, SLA, and ceramic 3D printers cost tens of thousands of dollars, making them a major investment for dental practices.
- Software & Training Required: Clinicians and technicians must be trained in specialized CAD software, increasing the learning curve and implementation time.
4. Regulatory & Biocompatibility Concerns
Since 3D-printed dental restorations and implants are placed inside the mouth, they must meet strict regulatory standards for biocompatibility. This includes FDA, CE, and ISO certifications, ensuring that printed materials do not cause adverse reactions or long-term complications. Additionally, cross-contamination risks must be minimized, requiring strict sterilization procedures for 3D-printed surgical guides and implants.
- Material Certification is Required: All 3D-printed materials used in dentistry must be FDA and CE approved, adding regulatory hurdles before clinical use.
- Cross-Contamination Risks: Strict sterilization procedures must be followed when using 3D-printed surgical guides, dentures, and implants, as improper handling could lead to infection risks.
Emerging Trends & Future of 3D Printing in Dentistry
Despite current challenges, ongoing research and technological advancements are driving the next generation of 3D printing innovations in dentistry.
Future Developments in 3D Printing for Dentistry
As 3D printing technology continues to evolve, new innovations are pushing the boundaries of speed, material quality, and automation. Emerging technologies such as Continuous Liquid Interface Production (CLIP), Lithography-Based Ceramic Manufacturing (LCM), 4D Printing, and AI-driven automation are expected to further revolutionize dental workflows.
Continuous Liquid Interface Production (CLIP) for Faster Printing
Traditional layer-by-layer 3D printing can be time-consuming, especially for high-precision dental applications. CLIP technology eliminates this delay by using an oxygen-permeable window, allowing for continuous printing without visible layer separations. This results in faster production speeds and superior surface quality, making it ideal for crowns, aligners, and dentures.
- 10x Faster Print Speeds: CLIP significantly reduces printing time, allowing dentists to produce restorations within minutes.
- No Visible Layer Lines: The seamless printing process eliminates step lines, providing a smoother, more natural-looking finish.
Lithography-Based Ceramic Manufacturing (LCM) for Zirconia Printing
Zirconia is one of the strongest and most aesthetic materials used in dentistry, but until recently, it could only be milled, not printed. LCM technology now allows for direct 3D printing of zirconia crowns and bridges, opening the door for high-strength, highly aesthetic restorations in additive manufacturing.
- Stronger than Traditional Resins: 3D-printed zirconia is wear-resistant, highly durable, and biocompatible, making it an excellent alternative to milled ceramics.
- Precision Similar to Milling: LCM technology ensures accurate fits, reducing the need for extensive post-processing or adjustments.
4D Printing: The Next Frontier in Orthodontics
4D printing is an advanced form of additive manufacturing that utilizes smart materials capable of changing shape over time in response to external stimuli such as temperature, pressure, or moisture. In dentistry, this could revolutionize orthodontics by creating self-adjusting appliances that adapt dynamically to a patient's needs.
- Self-Adjusting Aligners: Future orthodontic aligners could be designed to automatically shift as teeth move, reducing the need for multiple aligner sets.
- Dynamic Dental Splints: 4D-printed splints and nightguards could adjust their stiffness based on patient needs, providing customized bite correction without manual intervention.
AI-Driven 3D Printing & Automation
Artificial intelligence (AI) is rapidly transforming the dental industry, particularly in 3D printing workflows. AI-powered software solutions are helping automate prosthetic design, material optimization, and real-time quality control, reducing human error and production time.
- Predictive Modeling for Restorations: AI can analyze intraoral scans and CBCT data, automatically generating optimized prosthetic designs based on a patient’s specific needs.
- Automated Quality Control: AI-powered real-time monitoring systems can detect printing defects and material inconsistencies, ensuring consistent high-quality results.
Conclusion: The Future is Digital
3D printing is no longer a futuristic innovation—it is already redefining the dental industry by enhancing efficiency, precision, and patient outcomes. As dental practices continue to adopt additive manufacturing, the workflow becomes faster, more cost-effective, and highly personalized, leading to a better experience for both dentists and patients.
- Custom, patient-specific treatments are now a reality: Dentists can create restorations, implants, and orthodontic devices tailored to individual patients with unmatched accuracy.
- Faster production means fewer clinic visits and greater efficiency: Same-day restorations, digital workflows, and automated production reduce patient wait times and increase clinic productivity.
- Advancements in materials and AI will continue to expand the possibilities: From printable zirconia crowns to AI-driven design automation, future developments will push the limits of what’s possible in digital dentistry.
As 3D printing technology continues to evolve, dentists who embrace digital workflows will gain a competitive edge, offering faster, more precise, and cost-effective solutions. The future of dentistry is digital, patient-centered, and powered by additive manufacturing—and the time to adopt it is now.